Written by: Dr. Stephanie Mulick, O.D.
What are Flashes and Floaters?
If you have ever experienced a flash of light or spots in your vision it can be pretty alarming. I have experienced these symptoms on multiple occasions; and even as an Optometrist it can be a little scary.
Flashes and floaters can be a sign of a retinal tear or retinal detachment both of which require immediate attention.
If you ever experience flashes and/or spots in your vision get in to your nearest eye doctor for a Dilated eye exam.
Often, this can just be symptoms of an ocular migraine; however, if it is a retinal tear or detached retina, the quicker it is repaired the more likely you are to maintain good vision.
Retinal detachments can be treated and the sooner it is treated the better the visual outcome.
So don’t hesitate, if you experience flashes of light or spots in your vision call you eye doctor right away.
Quick Lesson on the Anatomy of the Eye
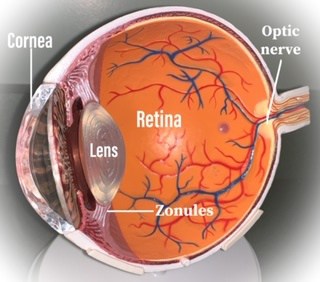
To understand flashes and floaters it is important to have an understanding of basic ocular anatomy. The eyeball consists of an anterior segment including the cornea, iris and lens and a posterior segment including the vitreous humor, the retina and the optic nerve.
The vitreous humor is composed of a transparent gel-like substance that fills the space in the eyeball between the lens and the retina, this helps to maintain the structure of the eye by providing shock absorption and support to the retina. The vitreous humor must be clear so that light can pass through it. According to a Caltech thesis, the vitreous humor is ~ 99% water and 0.9% salts (and) 0.1% divided between protein and polysaccharide components.”
The vitreous is enclosed in a clear membrane called the hyaloid membrane, which is attached to the retina in several areas.
As we age, the vitreous humor becomes more liquid, a process termed syneresis. Syneresis of the vitreous humor can cause it to shrink and collapse as well as pull away from the retina. This process can cause us to perceive floaters or wispy shadows in our vision and sometimes flashes of lights, due to pulling on the retina.
The separation of the vitreous humor from the retina is called a Posterior Vitreous Detachment (PVD).
Causes of Posterior Vitreous Detachment (PVD) and Retinal Detachment:
- Advanced age
- Trauma
- Cataract surgery (click here to learn about Cataracts)
- Yag laser Posterior capsulotomy
- Myopia (near-sighted) (click here to learn about myopia)
- Diabetes (click here to learn about Diabetes and the eye)
- Posterior Vitreous Detachment in the other eye
- Ocular inflammation
Symptoms of Posterior Vitreous Detachment:
- Flashes of light: usually intermittent
- Floaters: dark or grey shadows that may look like wispy lines, spider webs, dots or shapes
- Visual field (peripheral vision) defect
Complications of Posterior Vitreous Detachment:
- Persistent Floaters
- Retinal hole
- Retinal tears
- Retinal Detachment
- Macular hole (a hole of the macula of the retina, which provides central vision would cause a sudden decrease in central vision)
As the vitreous humor liquifies (syneresis), there is an increased risk for floaters, retinal holes or retinal detachments. It is very important to see your Eye Doctor as soon as you start seeing flashes or floaters. Your Eye Doctor will perform a series of tests including a dilated eye exam to view the vitreous and retina.
As the vitreous humor pulls away from the retina it can cause a retinal hole or tear. In some cases, a Retinal Detachment can occur which commonly presents with floaters, flashes and the perception of a curtain draping over one’s vision.
Symptoms could include floaters that don’t go away, distorted, blurry vision or a curtain over the vision.
Treatment of Floaters:
- Observation: With time the symptoms of floaters do usually improve and do not need treatment.
- Vitreolysis: with the use of a Yag laser, a Doctor can break up the floaters into smaller fragments making them less visible.
- Vitrectomy: A vitrectomy is defined as the removal of the vitreous humor.
Any surgical treatment of vitreous floaters come with possible side effects including:
- cataract formation
- pitting of an intraocular lens in a patient who has already had cataract surgery
- Increased eye pressure
- retinal tear or detachment
Symptoms of Retinal Tear, hole or Detachment:
- Flashes of Light (usually in one eye)
- Persistent floaters or increase in floaters
- Curtain-like shadow
- Peripheral vision defect
- Distorted or blurry vision
Treatment of Retinal holes, tears or Retinal Detachment:
- Observation: If asymptomatic, treatment may not be necessary and close observation would be recommended.
- If a patient is symptomatic, treatment with laser or cryotherapy is recommended.
- If the tear is large or a patient presents with a retinal detachment immediate surgical intervention is required and would be performed by a Retinal specialist.
Procedures for Retinal detachment repair:
Depending on the location and severity of the Retinal detachment your Retinal specialist will decide what the best treatment option for you will be.
- Laser photocoagulation: use of a laser to reattach the retina into place.
- Cryotherapy (freezing): creates scar tissue to keep the retina intact.
- Vitrectomy: removing the vitreous and replacing it with an optically clear and biologically inert substance such as gas or silicone oil. It is often required to lie face down for up to 2 weeks following a vitrectomy to ensure that the retina stays in place. Silicon oil will eventually need to be surgically removed whereas the gas bubble will absorb and our eye will naturally replace it with its own intraocular fluid.
Complications after Retinal detachment surgery:
- An increase in Intraocular Pressure (IOP) can lead to Glaucoma.
- Cataract formation
- Secondary Retinal Detachment: can occur when the gas bubble absorbs or the silicon oil is removed around 3-6 weeks after surgery.

Ocular Migraine (Scintillating scotoma or Visual aura):
Ocular Migraines are also known as scintillating scotoma or visual aura.
Symptoms of Ocular Migraine
Symptoms of an ocular migraine can include brief vision loss or perception of white or dark areas obstructing the vision and sometimes moving into the peripheral vision.
I have personally experienced ocular migraines that are usually accompanied by a migraine headache.
Not everyone who experiences ocular migraines have headaches; however, it is not uncommon for a headache to precede the visual aura.
Ocular Migraine Causes
Ocular migraines can be caused by vascular constriction or vasospasm of the blood vessels that lead to our eyes.
There is also a genetic predisposition; a family history of ocular migraine can increase your risk of experiencing them too.
Ocular migraine triggers (here are the most common triggers):
- Hormone changes or birth control pills
- Medication side effects
- Dehydration
- Alcohol or hang-over
- Stress or anxiety
- Lack of sleep
- Blood pressure changes
- Fermented foods
- Caffeine (a change from what you are used to; either too much or not enough)
- Chocolate
- Weather changes
- Nitrates (a preservative found in processed meats like deli meat and hotdogs)
- MSG (a seasoning most often found in processed foods)
- Bright lights
- Loud noises
Treatment of Ocular Migraine:
Usually, there is no need for medical treatment of ocular migraine if you experience them infrequently.
If you experience ocular migraines frequently with an unknown trigger it would be best to consult your primary care physician.
It often helps to keep a record of any trigger you encounter prior to experiencing an ocular migraine to try to narrow down the cause and avoid it in the future.
You should never ignore visual disturbances, especially if you experience flashes, floaters or vision loss, see your eye doctor immediately. It is very important not to ignore your symptoms or hope that they get better.
5 Causes of Flashes and Floaters:
- Ocular migraine
- Posterior Vitreous Detachment (PVD)
- Retinal Detachment (RD)
- Retinal Hole
- Retinal Tear
Conclusion:
Flashes and floaters are not to be taken lightly. If you experience flashes and floaters make sure to contact your nearest Eye Doctor.
Most of the time Flashes and Floaters are caused by a Posterior Vitreous Detachment, which usually does not require treatment and symptoms often subside. However, flashes and floaters can be a sign of more serious retinal complications such as retinal or macular holes, retinal tears or retinal detachments. At which point surgical repair may be necessary.
As far as a prognosis, the sooner you are treated, the better the visual outcome. So do not delay, schedule your eye exam immediately if you are experiencing flashes or floaters.


This was very informative and helpful! Thank you!
Thanks Cheyanne, Glad I could help!
An outstanding share! I have just forwarded this onto a coworker who was doing a little research on this. And he in fact ordered me lunch because I found it for him… lol. So let me reword this…. Thanks for the meal!! But yeah, thanx for spending some time to discuss this subject here on your web page.
Great info. Lucky me I discovered your website by chance (stumbleupon).
I’ve book marked it for later!
With havin so much written content do you ever run into any issues of plagorism or copyright infringement?
My blog has a lott off unique content I’ve either created myself or outsourhed but iit lookjs like
a lot of it is popping iit up all ofer the internet without mmy agreement.
Do you know any solutions to help stop content from being ripped off?
I’d definitely appreciate it.
Asking questions are genuinely fastidious thing if you are not understanding something totally, but this
article presents nice understanding even.
I really enjoy examining on this site, it holds great blog posts.
Dalam beberapa tahun terakhir, produk slot online telah
tumbuh menjadi salah satu rekreasi digital paling diminati di
Indonesia.
Kalau bicara soal jagat slot online, biasanya kita langsung teringat pada penampilan warna-warni, suara putaran gelung,
dan kejutan kecil yang tiba-tiba muncul saat simbol-simbol itu sejajar.
Trong nền văn hóa giải trí hiện đại, JAV đã trở thành một phần không thể thiếu
trong cuộc sống giải trí của nhiều người.
Một trong những trang web nổi bật trong lĩnh vực này chính là Kusex.
La falta de apoyo estructural también afectó la
viabilidad de muchas operaciones.
Buat lo yang udah lambat main slot online, pasti pernah ngalamin momen ngeselin:
mau login, eh web utama tiba-tiba nggak mampu dibuka.
Kadang kena memutus, kadang error random, kadang emang nasib
lo lagi kurang hoki aja.
I’ve been exploring foor a little forr any high quality articles or blig
postss on this sort of house . Exploring iin Yahoo I
at last stumbled upon this site. Reading this info So i’m glad to show
that I have an incredibly good uncanny feeling I discovered exactly what I needed.
I so much no doubt will make sure to don?t fail too remember
this site and give it a glance on a relentless basis.
Wow! This blog looks just like my old one! It’s on a completely different topic but it has pretty much the same page layout and design. Excellent choice of colors!