Written by: Dr. Stephanie Mulick, O.D.
Diabetes:
There are two types of Diabetes:
- Type 1 or insulin-dependent, once referred to as juvenile Diabetes, usually presents before the age of 30.
- Type 2 also known as non-insulin dependent is usually diagnosed after the age of 30.
What is Diabetes?
Diabetes occurs when our blood glucose (sugar) becomes elevated also known as hyperglycemia. Insulin is a hormone that is produced by the beta cells of the pancreas. In a diabetic patient, the pancreas does not produce enough insulin or sometimes doesn’t produce insulin at all. This is a problem because insulin helps get glucose (sugar) from ingested food or liver stores into our cells to produce energy. If the glucose is unable to get into our cells because of a lack of insulin then it stays in our bloodstream causing high blood sugar.
High blood glucose can cause vascular damage leading to Complications:
- Diabetic Retinopathy: Leading cause of blindness in patients age 20-65 years old
- Neuropathy: nerve damage
- Diabetic Nephropathy: kidney damage
- Heart disease
- Stroke
Our main source of glucose comes from Carbohydrate-rich foods
Patients with Diabetes should limit the following foods:
- Bread and grains: rice, wheat, oats and flour (including gluten-free)
- Some fruits: bananas, mangoes, dates, raisins
- Some Vegetables: Potatoes, corn, beets
- Pasta
- Cereal
- Sugar, Honey or Agave (look at the packaging for added sugar)
- Milk
- Chips and crackers (including gluten-free)
- Juice
- Beer

Blood Sugar Measurements:
- Fasting blood glucose: Blood sugar after not eating for at least 8 hours.
- Postprandial or after a meal: Blood glucose within 2 hours of eating.
- Hemoglobin A1c (HbA1c or A1c or Glycated haemoglobin): Hemoglobin in our red blood cells carry oxygen through the bloodstream to supply oxygen to our cells throughout our body. The term glycated haemoglobin means haemoglobin that is bound to glucose (ie: blood sugar/blood glucose).
Some people consider themselves borderline Diabetic or Pre-diabetic because the blood glucose has not reached the high levels; however, it is still important to know the even pre-diabetic patients can have similar health risks as Diabetic patients.
Blood Glucose Level Chart
| Classification | Fasting (at least 8 hours) | Postprandial Blood Sugar (after meal) | A1c |
| Normal | 70-100 mg/dL | 70-140 mg/dL | Less than 5.7 |
| Prediabetes | 101-125 mg/dL | 141-200 mg/dL | 5.7-6.4 |
| Diabetic | 125 mg/dL or higher | 200 mg/dL or higher | 6.5 or higher |
Common Symptoms of Diabetes:
- Frequent urination
- Increased Thirst
- Increased hunger (even after eating)
- Increased Fatigue
- Fluctuations in vision
- Slowed wound healing
- Numbness or tingling in hands and feet
Risk Factors for Type 1 and Type 2 Diabetes:
Type 1 Diabetes risk factors:
- Family history
- Exposure to a viral illness
- Living further from the equator or colder climates
Type 2 Diabetes risk factors:
- Overweight: BMI greater than 25
- Lack of exercise
- Family history
- Gestational diabetes: Diabetes when pregnant
- Polycystic ovarian syndrome
- Hypertension (high blood pressure
- Low levels of HDL (high-density lipoprotein)
- High levels of triglycerides
Diabetic Retinopathy:
Diabetic Retinopathy is the leading cause of blindness in the US population ages 20-65.
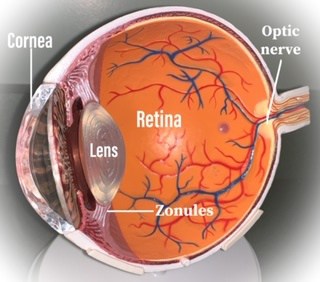
The eye is the only organ in our body where Doctors can directly view the blood vessels. This is particularly important when evaluating Diabetes, high cholesterol and high blood pressure.
Diabetes affects the blood vessels, so having a yearly dilated eye exam is extremely important when it comes to preserving vision.
Diabetic Retinopathy Classifications:
There are 2 classifications of Diabetic Retinopathy:
- Nonproliferative Diabetic Retinopathy: which can be classified as mild, moderate or severe.
- Patients with mild NPDR usually present without symptoms and do not require treatment other than proper blood sugar control.
- Moderate and Severe NPDR should be watched closely with eye exams every 3 months because of the high risk of Proliferative Diabetic Retinopathy.
- Treatment for NPDR is usually not necessary. However, depending on the severity of your Retinal specialist may choose to do a minimally invasive laser called photocoagulation to help prevent further retinal damage.
2. Proliferative Diabetic Retinopathy
- This is an advanced stage of Diabetic retinopathy in which the signs of retinal hypoxia will be apparent including neovascularization and severe retinal hemorrhages which cause loss of vision.
- At this stage, treatment is urgent and may include laser, vitrectomy or medication injection into the eye depending on the severity.
If you have been diagnosed with Diabetes or you are taking Metformin, make sure to see your eye doctor at least once per year for a dilated eye exam.
Diabetic Retinopathy Signs:
- During your dilated eye exam the Doctor may see arteriole changes, microaneurysms, hemorrhages, oedema, exudates (seen as yellowish spots in the retina which are made up of lipids that leak out of damaged capillaries) and microvascular abnormalities.
- Some patients present without symptoms or may complain of vision fluctuations.
- In moderate to severe cases of Diabetic Retinopathy, your Eye Doctor will refer you to a Retinal specialist for special testing including: Fluorescein Angiography (FA), a test to view microvascular leakage, Macular OCT (Optical Coherence Tomography) tests for retinal oedema. Depending on the severity the Retinal specialist may need other tests to view the retina properly.
Symptoms that could present with Diabetic Retinopathy:
- Dark spots in your vision
- Vision fluctuations
- Loss of vision
Treatment of Diabetic Retinopathy (DR):
- Tight control of blood glucose levels
- Tight blood pressure control
- Depending on the severity: Laser Photocoagulation may be required
- Occasionally a vitrectomy is necessary
- Depending on severity: medicated injections into the eye may be necessary
The more severe the Diabetic Retinopathy the more likely the need for treatment with Laser or injections will be. Maintaining stable blood glucose levels and having annual dilated eye exams will help to prevent the need for retinal surgery or injections.
Complications include Cataracts and neovascular glaucoma.
Risk factors for Diabetic Retinopathy (DR):
- Duration of diabetes: the longer someone has diabetes it is more likely to develop DR.
- Poor blood sugar control
- Pregnancy
- Hypertension (high blood pressure)
- Nephropathy (renal or kidney disease)
- Smoking
- Obesity
- Hyperlipidemia (high cholesterol)
Blood sugar control:
The best treatment for Diabetes is blood sugar control.
- Monitor your blood sugar levels: So many of my patients do not know their own blood sugar levels. This is such an easy test that can tell you so much. Check the table above for blood sugar levels.
- Exercise regularly: even a 20-30 minute daily walk can improve your blood sugar.
- Limit foods high in carbohydrates
- Increase consumption of fiber: Use the ratio of Carbohydrates divided by fiber equals 10 or less. Carbohydrates ÷ Fiber ⪳ 10. This is a great way to shop for groceries especially when purchasing packaged foods. Fiber has many health benefits, especially when it comes to Diabetic patients. Studies have shown that diets high in fiber can aid in blood sugar control.
- Eat more vegetables: Filling your plate with vegetables will increase your fiber intake.
- Consume cinnamon especially in the form of Ceylon cinnamon, which is less toxic than traditional cassia cinnamon. Cinnamon has been shown to decrease blood sugar levels.
- Limit packaged and processed foods.
- Be mindful of when you eat. The MMC pathway, also known as the Migrating motor complex is the process of digestion that occurs in between meals. In a study titled: “Upper gastrointestinal sensory-motor dysfunction in diabetes mellitus” in the World Journal of Gastroenterology motility patterns were abnormal in Diabetic patients. The MMC pathway starts 2-3 hours after consuming any calories. Taking longer breaks between calorie consumption allows the MMC pathway to move food through the digestive system.
- Drink water regularly throughout the day
- Limit stress: I know this is easier said than done, but stress can stimulate the production of the hormones: glucagon and cortisol, both of which increase blood sugar levels.
- Sleep regularly: staying on a regular sleep schedule can help to control your hormones and blood sugar levels.
Conclusion:
Diabetes is a life-threatening and sight-threatening disease. If you are looking to reduce your risk for vision complications as well as systemic complications that accompany Diabetes make sure to follow the advice of your Doctors and have an eye exam at least once a year unless advised otherwise by your physician. Blood sugar control is of the highest importance when it comes to decreasing your risk of Diabetic complications. Make sure to check your blood sugar regularly and avoid sugary, high carbohydrate foods and exercise daily.