Written By: Dr. Stephanie Mulick, O.D.
The 4 refractive eye surgery options in 2025 are:
- LASIK
- PRK
- ICL (implantable Collamer lens)
- Clear lens extraction with PanOptix, Vivity, or Light Adjustable Lenses (LAL)
So you have been wearing glasses for quite some time now, in fact, you are dependent on glasses and have been considering Refractive surgery, so you can be done with glasses for good. Well, let’s look at the facts and determine if and which surgery would best fit your needs.
Having eye surgery should not be taken lightly, after all, we’re talking about your vision here.
I personally have worn glasses since I was 5 years old, and started wearing contact lenses at age 13. Overall, I haven’t had any issues with glasses or contact lenses, and even as an Optometrist, I never really considered surgery for myself.

Refractive Error (Myopia, Hyperopia, Astigmatism and Presbyopia)
Let’s start off by talking about the differences between myopia (near-sighted), hyperopia (far-sighted), Astigmatism (irregular cornea or lens shape), and presbyopia (loss of focus after age 40).
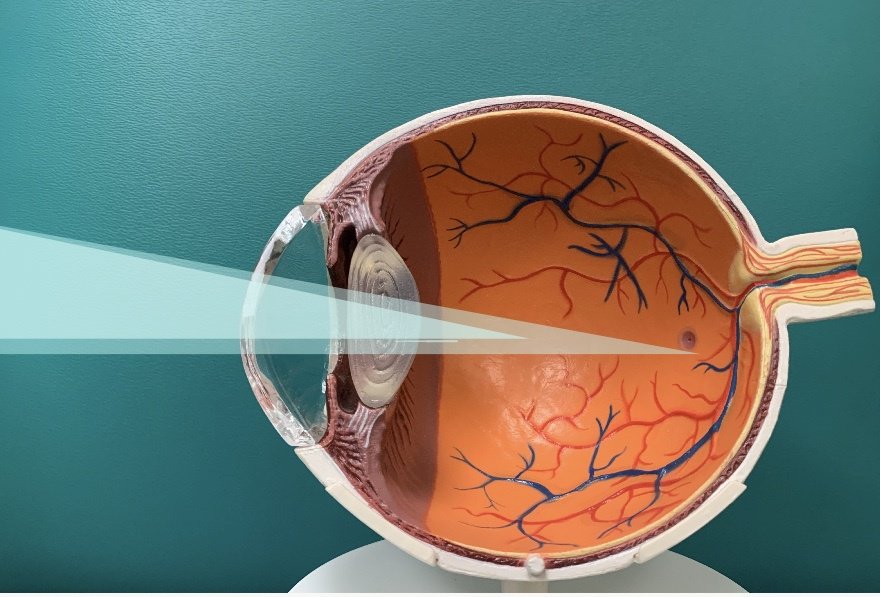
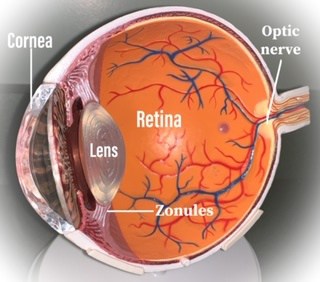
A refractive error is a term used to describe the way light is bent when it comes into your eye. Refraction means the bending of a wave, in the case of the eye we are referring to bending light waves. An Optometrist will perform a Refraction (the dreaded “Which is clearer 1 or two.” test) to determine the power of the lens required to get our patients clear vision. The lens power is measured in quarter step Diopters.

Myopia (Near-sighted)
A near-sighted eye is a longer eye, which means that when the light from a distant object comes into the eye, instead of focusing directly onto the retina it focuses in front of the retina, causing a blurry image. When looking at a near object the light moves closer to the retina, making near objects clearer for a near-sighted eye.
A myope or near-sighted eye is able to see near objects, but distant objects are blurry.
Glasses for a myopic eye would have a minus powered lens, for example, -2.00 Diopters.

Hyperopia (Far-sighted)
Hyperopia or far-sighted means that the individual has a shorter eye and light focuses behind the retina. This makes it more difficult to focus on near objects. Even though a far-sighted eye sees better at a distance than up close, they still find improvement in distant vision with glasses and the near vision can be much improved with glasses. It is not uncommon for a hyperopic (far-sighted) patient to complain of eye strain or headaches after prolonged near work (ie: computer, phone, or reading).
Glasses for a Hyperopic eye would have a plus-powered lens, for example, +2.00 Diopters.
Presbyopia
Presbyopia means loss of focus or accommodation. The lens in our eye adjusts our focal point by accomodating or changing shape to move the light onto the retina when we look up close. As we advance in age the natural crystalline lens of our eyes becomes thicker and more difficult to accommodate the light. This causes us to lose the ability to focus on near objects. Now, a near-sighted eye will see up close better without glasses, but for everyone else, reading glasses will become a progressive need.
One of my patients explained presbyopia as “after 40 vision”. I thought that was a cute way of saying it, but he is true, presbyopia does usually start in our 40’s and progresses until about age 60.
Presbyopia causes us to need reading glasses, that is unless you are near-sighted and just remove your glasses to see up close. But for someone who is perfectly corrected to see clearly at a distance, when they become presbyopic the need for reading glasses will progressively increase with time until about age 60 at which point it doesn’t tend to get worse.
After the age of 60, it is more common to start seeing the development of cataracts that can affect the vision causing glare and halos at night and the need for more light especially when reading. Cataract development will progress until eventually cataract surgery is needed (review my post on cataracts for more information).
Glasses for Presbyopia would have an ADD power which is an additional reading power that is added to the power of lens needed to see at distance.
Astigmatism
The term astigmatism means that there is an irregularity to the shape of the eye causing light to bend in many directions. The irregularity of the eye can be caused by corneal astigmatism or lenticular astigmatism or a little of both.
Corneal Astigmatism means that the cornea or front of the eye is not perfectly spherical (round). Lenticular astigmatism means that the lens inside of the eye is irregular. Both types of astigmatism cause vision distortion and blur.
Without getting deep into optics, a non-astigmatism prescription for glasses is called spherical and would look something like this: -2.00DS (Diopters sphere) or -2.00sph (sphere). Glasses that correct astigmatism would have a number called the cylinder and axis and look something like this: -2.00 -1.25 x 180. The middle number is the cylinder and the third or last number is the axis, this is the part of your prescription that corrects your astigmatism.
Refractive Surgery Options to Correct Blurry Vision
Wouldn’t it be great to get rid of glasses and contact lenses for good? Being dependent on glasses and contact lenses can be a bit scary, especially if there were ever a major disaster (Heaven Forbid).
As the title of this post suggests, I am going to review 4 surgical options that could improve your vision.
LASIK (Laser-Assisted In-Situ Keratomileusis)
Let’s start with LASIK. LASIK is well-known and highly effective. According to LASIK World Literature Review: Quality of Life and Patient Satisfaction in Ophthalmology Volume 116, issue 4, “the overall patient satisfaction rate after primary LASIK surgery was 95.4%.” LASIK is a laser-assisted procedure that creates a hinged flap on the cornea, then the tissue below the flap is ablated or removed by the laser and the flap is then put back into place.
The term LASIK was first coined by Dr. Ioannis Pallikaris in 1990. The first U.S. clinical trials were performed in 1991. And reached its height of popularity in 2007, with about 1.5 million surgeries performed. According to the eye care data source Market Scope, 604,000 LASIK surgeries were performed in 2015.
The decline in LASIK’s popularity could be a result of new technologies in refractive surgeries such as refractive cataract surgeries or clear lens extraction, implantable Collamer lens (ICL), or possibly the economic decline of 2008. Other contributing factors can be that the fashion industry has brought glasses from geek to chic as well as new advances in contact lens technology.
LASIK is a great option for patients ages 18-40, as long as your glasses prescription has not been changing significantly throughout the years. It is best to have LASIK when you have had stable vision for a few years. Patients over the age of 40 can still be good candidates for LASIK; however, they need to keep in mind that they may need reading glasses after due to presbyopia. As stated earlier, presbyopia makes it difficult to focus on near objects. When treating a presbyopic eye with LASIK the option of monovision will be discussed.
Monovision allows one eye, usually the non-dominant eye to see near objects (near-sighted) and the other, dominant eye to see distant objects. This is done to avoid the need for reading glasses. Some patients who have been dependent on glasses for a long time are willing to use reading glasses after surgery, in which case, both eyes can be corrected for distance.
If you choose to have monovision, it would be recommended to try it first using monovision contact lenses.
Risks can include:
- Vision problems, such as poor night vision, glare, halos and haze
- Dry eye syndrome
- Photophobia (light sensitivity)
- Incomplete or inaccurate vision correction
- Infection
- Scarring
- Corneal ectasia (steepening of the cornea)
Corneal ectasia is a rare, but serious complication of LASIK. With advanced technologies and current procedures, this is an extremely rare side effect.
Prior to LASIK, patients will be evaluated as to whether they are candidates for LASIK including risk assessment for corneal ectasia. This is assessed by using corneal topography and thickness measurements. If LASIK is not an option it is possible that you may still qualify for PRK (photorefractive keratectomy).
PRK (photorefractive keratectomy)
PRK is similar to LASIK without the creation of a corneal flap. This can be beneficial in patients with a thin cornea or high refractive error who may not be candidates for LASIK. Since there is no corneal flap created, the healing process can be slightly more painful. However, with the use of bandage contact lenses, most patients say the pain is minimal and lasts for just a few days.
Just like LASIK, monovision can be an option if one desires.
Risks of PRK can include:
- Dry eye syndrome
- Vision problems, such as poor night vision, glare, halos and haze
- Incomplete or inaccurate vision correction
- Photophobia (light sensitivity)
- Infection following surgery
Overall, PRK is safe and effective at treating most refractive errors.

Implantable Collamer lens (ICL)
An ICL is a lens that is implanted behind the iris, in front of the natural crystalline lens of the eye to provide clear vision. Just like LASIK and PRK, presbyopic patients would have the option of monovision. Because the lens is taking up space in the eye it is important for the surgeon to perform special measurements to determine if there is adequate space in the eye. They will also perform a small laser incision into the iris to prevent an increase in intraocular pressure (IOP).
Risks of ICL:
- Development of cataract (According to the study titled Implantable Collamer Lens for Myopia: Assessment 12 Years After Implantation, there was 13.88% risk of cataract development postoperatively
- Increased intraocular pressure
- Retinal detachment – Less than 1 percent of patients in the clinical studies for both the Verisyse™ phakic IOL and the Visian ICL™ were affected by retinal detachment. It should be noted, however, that the occurrence of retinal detachment increased as the degree of myopia increased.
- Loss of vision: with any eye surgery this could be a risk factor, but it is extremely rare.
Refractive Clear lens extraction
Because of the limitations of monovision in presbyopic patients, a clear lens extraction may be a better option. Clear lens extraction is the same procedure that is done to remove a cataract, but in this case, the crystalline lens is clear instead of cloudy. With the advent of advanced intraocular lens implants (IOLs) like the PanOptix trifocal lens, the Vivity extended depth-of-focus lens, and the Light Adjustable Lens (LAL), patients can experience a greater depth of focus and better overall visual outcomes.
These multifocal and extended depth-of-focus lenses allow for distance, intermediate, and near vision in both eyes simultaneously, reducing dependence on reading glasses. The Light Adjustable Lens offers the ability to fine-tune vision postoperatively using UV light adjustments tailored to the patient’s visual needs. The choice between PanOptix, Vivity, and LAL would be discussed thoroughly during your cataract evaluation based on your visual needs and lifestyle.
Additionally, femtosecond laser-assisted surgery (a highly precise, bladeless laser used to make corneal and lens incisions) can be used in this procedure to create highly precise incisions and lens fragmentation, which may improve visual outcomes and recovery time. This bladeless laser approach adds a new level of accuracy compared to traditional manual techniques.
Having clear lens extraction will prevent you from ever developing a cataract because the natural crystalline lens will be removed and replaced with a new biocompatible lens that corrects your vision.
Another benefit of refractive clear lens extraction is that the corneal tissue is left intact except for a self-sealing 3mm incision that is created to remove the natural crystalline lens and replace it with an intraocular lens.
As with every surgery, there are always risks to be aware of. Cataract surgery is one of the safest and most effective vision-correcting procedures, which is why more than 3 million cataract surgeries are performed each year in the U.S.
Complications following refractive clear lens extraction are very rare and usually not serious.
Ensuring that you follow up with your eye doctor and use the prescribed eye drops will help ensure proper healing of your eyes after cataract surgery.
This list of postoperative complications below came from my post on cataracts (here is the link).
Some postoperative complications of clear lens extraction are:
- Posterior capsular opacification (PCO): This is a prevalent condition that can be easily treated with a quick YAG laser. A posterior capsular opacification occurs when the natural posterior capsule of the eye, which is located behind the new IOL, becomes cloudy. The Yag laser is a quick and effective treatment for removing the cloudy capsule, allowing for improved vision. Many patients with Posterior capsular opacifications experience a decrease in vision similar to the effects of the original cataract. A PCO can develop any time after Cataract surger,y from immediately to several years later.
- Ocular infection: After cataract surgery, it is very important to follow up with your eye doctor as directed. Ocular infection after cataract surgery is sporadic, with an incidence ranging from 0.13% to 7%, as stated in the Current Opinion of Ophthalmology journal.
- Retinal detachment occurs when the sensory retina is pulled away from its normal location. Patients may experience flashes of light, floaters, or shadows in their vision, or even a curtain-like obstruction over their vision. If you experience any of these symptoms, please see your nearest eye doctor immediately.
- Lens Fragments: Some complicated cataract surgeries result in pieces of cataract left behind. If the pieces are small, there is usually no concern; large pieces of lens fragments may require additional surgery.
- Inflammation: it is normal to have inflammation after surgery, which is why you will be required to use steroid and anti-inflammatory eye drops. Excessive inflammation may require more aggressive treatment.
- Dislocated IOL: In extremely rare cases, if the IOL falls out of position and into the back of the eye, another surgery would be necessary.
- Floaters: You may see dark spots in your vision that move around. This is usually not a serious issue, but it should be addressed with your eye doctor.
- Retinal fluid or macular edema: The use of NSAID eye drops postoperatively has been shown to reduce this risk. If your vision becomes blurry or wavy, consult your doctor for an evaluation.
- Ocular hypertension (High intraocular pressure)
- Photophobia: It is not uncommon to become light-sensitive after cataract surgery due to more light entering the eye. It is recommended to always use sunglasses (preferably polarized) outside.
- Dysphotopsia: Some patients experience a dark or light area in their peripheral vision, which typically resolves within a few weeks.
- Temporary ptosis (lid droop): This is a rare side effect of cataract surgery that usually improves with time.
So what would I choose?
I started this post off by saying: I have personally worn glasses since I was 5 years old, and started wearing contact lenses at age 13. Overall, I haven’t had any issues with glasses or contact lenses, and even as an Optometrist, I never really considered surgery for myself. That was until just a few weeks ago.
Since I am not a candidate for LASIK, I would consider PRK or clear lens extraction as alternatives. With PRK, I would have to decide whether I want both eyes to see well for distance and wear reading glasses or opt for monovision. Whereas, with clear lens extraction, I may not need reading glasses except for very fine print or in dimly lit areas.
I am at the beginning stage of presbyopia (loss of focus) and have not done much of a monovision trial on myself to know if I would like it permanently. However, I would consider having improved distance vision and using reading glasses for computers and reading.
Most everyone gets a cataract eventually if they get to live a long life. So, clear lens extraction is one way to avoid the development of a cataract in the future.
Knowing how well my patients have done after the newest generation multifocal IOL for cataract surgery, I would also consider clear lens extraction, especially with the technology evolving so quickly.
Conclusion:
The 4 refractive eye surgery options in 2025 are:
- LASIK – Best for patients under 40 with stable prescriptions and healthy corneas.
- PRK – Great for thinner corneas or high prescriptions, with slightly longer healing.
- ICL (implantable Collamer lens) – Ideal for high myopes or those not suited to laser surgery.
- Clear lens extraction with PanOptix, Vivity, or Light Adjustable Lenses (LAL) – Excellent for patients over 45, offering multifocal solutions and the option to avoid future cataract surgery.
These all have risks and benefits associated with them. It is essential to consider your options and determine what would best suit your needs and lifestyle.


I really like what you guys are up too. Such clever work and
exposure! Keep up the terrific works guys I’ve incorporated you guys to
my blogroll.
Wonderful site you have here but I was curious about if you knew of any message boards that cover the same topics discussed in this article?
I’d really like to be a part of group where I can get
opinions from other knowledgeable people that share the same
interest. If you have any recommendations, please let me know.
Kudos!
Wonderful post however , I was wanting to know if you could write a litte more on this topic? I’d be very thankful if you could elaborate a little bit more. Cheers!
Do you have a spam issue on this blog; I also am a blogger, and I was wondering your situation; many of us have developed some nice procedures and we are looking to exchange methods with others, please shoot me an e-mail if interested.